About drjohnzhang
View all posts by drjohnzhang
A Celebrated Mini-IVF™ Protocol That Strategically Uses Low Dosages of Fertility Medication

 A celebrated Mini-IVF™ protocol is one that will increase your chances of pregnancy without the need for large dosages of costly fertility medications. Why does this matter? No longer do you need to produce an excessive number of eggs to achieve a successful pregnancy. Here’s the deal: The goal with a Mini-IVF™ protocol is to produce between 3 and 5 quality eggs per fresh cycle. The best part: Pregnancy success rates for Mini-IVF™ are comparable to Conventional IVF.
A celebrated Mini-IVF™ protocol is one that will increase your chances of pregnancy without the need for large dosages of costly fertility medications. Why does this matter? No longer do you need to produce an excessive number of eggs to achieve a successful pregnancy. Here’s the deal: The goal with a Mini-IVF™ protocol is to produce between 3 and 5 quality eggs per fresh cycle. The best part: Pregnancy success rates for Mini-IVF™ are comparable to Conventional IVF.
Mini-IVF™ Overview
Because lower dosages of fertility medications are prescribed to only produce 3 to 5 high quality eggs, the patient’s cost per Mini-IVF™ cycle is reduced. Bottom Line: The patient’s physical discomfort is lessened because her body is not forced into producing the typical 10 to 15 eggs reached in a Conventional IVF cycle.
Look: The Mini-IVF™ protocol in a nutshell.
- A fertility medication regimen to produce 3 to 5 quality eggs
- Cycle monitoring through ultrasound imaging and blood tests
- Surgical egg retrieval
- Fertilization of egg and sperm in vitro via (ICSI)
- Culture and monitoring of embryo(s) via EmbryoScope technology
- Grading and selection of quality embryo(s) for fresh transfer and/or future (FET)
- Single Embryo Transfer (SET)
Candidates for Mini-IVF™
Mini-IVF™ is the best treatment protocol for those women who have been:
- Diagnosed with blocked or damaged Fallopian tubes
- Diagnosed with Polycystic Ovarian Syndrome (PCOS)
- Diagnosed as having a risk of developing Ovarian Hyperstimulation Syndrome (OHSS)
- Diagnosed with a low ovarian reserve
- Diagnosed with cancer and are about to undergo treatment
Mini-IVF™ has also become the preferred treatment protocol for:
- Those patients who have failed multiple Conventional IVF cycles
- Those patients suffering from male-factor infertility
- Those patients wanting to reduce their costs of treatment
- Those patients wanting to reduce their risk of multiple pregnancy
- Those patients who don’t want to create excessive embryos due to religious reasons
- Those patients who want to reduce their use of injectable medications because of an aversion to needles
- Those patients who want to undergo another fresh IVF cycle immediately after a failed cycle
Mini-IVF™ Medications
Depending on the woman’s medical needs, an oral fertility medication – Clomid – is prescribed to gently stimulate her ovaries into producing multiple eggs. But there’s a catch. In some cases, three or fewer of injectable gonadotropins – Menopur – may be prescribed in combination with Clomid to encourage egg production. Finally, Synarel is delivered nasally 36 hours prior to surgical egg retrieval.
Downsides to Mini-IVF™
Unlike with Conventional IVF, Mini-IVF™ patients are less likely to have leftover embryos to cryopreserve for future Frozen Embryo Transfers (FET). Why does this matter? If a cycle fails, and multiple subsequent fresh Mini-IVF™ cycles are pursued, costs can add up to be greater than a Conventional IVF where multiple embryos are produced and can be cryopreserved.
Another risk of Mini-IVF™ is that a patient could end up producing unhealthy eggs that are not able to be fertilized. Or, the embryos produced in vitro may not be healthy for transfer.
Quality Eggs – Not Quantity of Eggs
Dr. John Zhang – founder and medical director of New Hope Fertility Center, developed the Mini-IVF™ with the goal of producing high quality eggs – not an excessive quantity of low quality eggs.
According to Dr. Zhang:
In many cases, someone who fails a conventional cycle will have better luck with lower stimulation protocol like Mini-IVF™ since it can produce higher quality eggs. – Dr. John Zhang
It is a case-by-case situation, but you should not assume that because one cycle fails, all treatment will. *** Studies show that women can have a higher success with lower stimulation over the course of multiple cycles. By trying another treatment, we have seen better success. – Dr. John Zhang
Celebrated Mini-IVF™ Doctor
It is important to work with a celebrated Mini-IVF™ Doctor having the experience required to design a customized treatment protocol meeting your personal needs. To schedule your initial consultation with Dr. John Zhang at New Hope Fertility NYC, call 917.525.5496.
The Summer Fertility Diet to Start NOW
 If you will be trying to get pregnant this summer – you should definitely think about what you’re eating. Why is diet important? Today, it is estimated that one in eight couples has difficulty conceiving and/or carrying a baby to full term. Look: A healthy diet will increase your chances of conceiving and help to support a healthy pregnancy.
If you will be trying to get pregnant this summer – you should definitely think about what you’re eating. Why is diet important? Today, it is estimated that one in eight couples has difficulty conceiving and/or carrying a baby to full term. Look: A healthy diet will increase your chances of conceiving and help to support a healthy pregnancy.
Summer Fertility Diet
Summer is a prime time for trying to get pregnant so you can give birth to a healthy baby next spring. Unfortunately, having a baby the natural way isn’t always easy and you must be more proactive in your quest for conception success.
Today, more women in their 30s and 40s are wanting to become first-time moms than their 20-something counterparts. What’s the real story? A Nurses’ Health Study found that women who followed a fertility diet had a 66 percent lower risk of ovulatory dysfunction. The participants in this study followed a recommended fertility diet.
- Plant-based foods
- Protein-rich foods
- Healthy fats
- A bit of full-fat dairy products
Bottom line: Nutrition and optimal fertility go hand-in-hand.
The DASH Diet
A fertility diet – known as the DASH Diet can improve your health, lower your BMI, and reduce your risk of PCOS. The DASH Diet – Dietary Approaches to Stop Hypertension – is a low-calorie diet helping to increase fertility in women. Women adhering to the DASH Diet can reduce BMI at a higher rate than those on a typical low-calorie diet.Read more: The Summer Fertility Diet to Start NOW
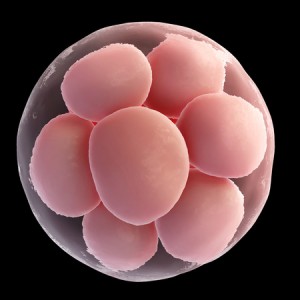
How Embryology is Key to IVF Pregnancy Success

 Expertise in embryology is key to IVF pregnancy success. Embryology is the study of an embryo from the first stage of fertilization through fetal development. High quality embryos have the highest chance of implantation into a woman’s uterine lining resulting in a successful pregnancy. After egg retrieval, one or two healthy embryos are transferred after a fresh IVF cycle. Excess embryos culturing in vitro are cryopreserved for future pregnancies through Frozen Embryo Transfers (FET).
Expertise in embryology is key to IVF pregnancy success. Embryology is the study of an embryo from the first stage of fertilization through fetal development. High quality embryos have the highest chance of implantation into a woman’s uterine lining resulting in a successful pregnancy. After egg retrieval, one or two healthy embryos are transferred after a fresh IVF cycle. Excess embryos culturing in vitro are cryopreserved for future pregnancies through Frozen Embryo Transfers (FET).
Embryology Roles in the IVF Process
- HRSS – High Resolution Sperm Selection
- ICSI – Intracytoplasmic Sperm Injection
- Assisted Hatching
- In Vitro Maturation
- EmbryoScope
Embryologists at New Hope Fertility Center choose the healthiest sperm to fertilize an egg in vitro. Cutting edge technology provides embryos culturing in vitro with an optimum environment for healthy development prior to fresh transfer and/or cryopreservation.Read more: How Embryology is Key to IVF Pregnancy Success
Check Out New Hope’s Egg Donation Program

 An egg donation program helps infertile couples grow their families through IVF technology. New Hope Fertility Center spearheaded the 21st century’s most acclaimed egg donation program. Many women donate their eggs at New Hope Fertility Center because they want to give the gift of life to other families. Our program has been created for the sole purpose of matching recipient couples with an optimum egg donor. We work closely with donors and recipients to ensure the process is smooth, confidential, and user-friendly.
An egg donation program helps infertile couples grow their families through IVF technology. New Hope Fertility Center spearheaded the 21st century’s most acclaimed egg donation program. Many women donate their eggs at New Hope Fertility Center because they want to give the gift of life to other families. Our program has been created for the sole purpose of matching recipient couples with an optimum egg donor. We work closely with donors and recipients to ensure the process is smooth, confidential, and user-friendly.
Egg Donation Program
Through New Hope’s egg donation program, you will be efficiently matched with an egg donor. Our egg donation coordinators carefully matched 100s of intended parents with egg donors to achieve a successful pregnancy. We help intended parents find egg donors with similarities in ethnicity and physical characteristics.
- For Donor Information
- For Recipients
- About Surrogacy using donor eggs
Egg Donor Qualifications
- Excellent medical and mental health
- Ages 18 to 28
- Local and out-of-state donors welcome
Candidates for Egg Donation Services
IVF using donor eggs is a proven method of successfully treating those who are unable to produce and/or use their own eggs to have a baby.
- Women who are unable to sustain a pregnancy
- Women suffering from unexplained infertility
- Women who have unhealthy eggs
- Women who are predisposed to passing on a genetic disease
- LGBTQ couples – especially same sex male couples unable to recruit a known-donor
IVF using donated eggs brings great hope and joy to the donor as well as the intended parents. Our egg donation program is renowned for providing egg from healthy young women who have been closely screened to ensure their physical and mental health.Read more: Check Out New Hope’s Egg Donation Program
New Hope’s Needle-Free IVF Protocol

 Since being introduced in the 1970s, Conventional IVF treatment has relied heavily upon high dosages of fertility medication – as many as 60 injections per cycle. Look: New Hope Fertility Center is the first program in the world to offer Needle-Free IVF. Why does this matter? It is now possible for women to undergo IVF without the need for injections.
Since being introduced in the 1970s, Conventional IVF treatment has relied heavily upon high dosages of fertility medication – as many as 60 injections per cycle. Look: New Hope Fertility Center is the first program in the world to offer Needle-Free IVF. Why does this matter? It is now possible for women to undergo IVF without the need for injections.
Revolutionary Breakthrough in IVF
Needle-Free IVF. We have achieved another first by introducing Needle-Free IVF. This revolutionary holistic IVF protocol eliminates the fear, pain, and anxiety many patients experience with injections and blood draws – while at the same time lessening the cost of fertility medications.
Needle-Free IVF
We are proud to offer our patients a new, simple and convenient Needle-Free IVF treatment protocol. The best part? This revolutionary IVF protocol eliminates the fear, pain, and anxiety many patients experience when having to inject fertility medications with needles. Our Needle-Free IVF protocol stimulates a woman’s ovaries into producing multiple egg follicles through the use of oral fertility medications. That’s not all. Hormone levels are measured through urine and saliva tests during a Needle-Free IVF cycle.
Needle-Free IVF Benefits
Through Needle-Free IVF, patients are able to administer hormone stimulation in a less-invasive manner.
- No shots
- No needles
- No injections
- No blood draws
Needle-Free IVF Protocol
Why Needle-Free IVF is patient-friendly.
- Improves patient safety
- Improves patient compliance with medication regimen
- Reduces possibility of error in medication administration
- Eliminates the risk of accidental needle sticks
How FET Can Improve Your IVF Pregnancy Success Chances
Freezing excess, quality embryos after a fresh IVF cycle will increase a couple’s chances of conceiving in the future. This is not even the best part. Through embryo cryopreservation technology, couples can avoid the financial and physical strain of undergoing multiple fresh IVF cycles. That’s not all. The pregnancy success rate for a Frozen Embryo Transfers (FET) is higher than a fresh transfer because a woman has the opportunity to wait until her uterine lining returns to an ideal state for embryo implantation.
Benefits of the Frozen Embryo Transfer (FET)
Through Frozen Embryo Transfer (FET), couples can try again – sooner than later – if their fresh IVF cycle fails. If the fresh IVF cycle is successful, the couple can undergo a FET at a time when they decide to have more children in the future.
Bonus Benefits of FET
- Couples can plan their family through gender selection
- Couples increase their chances for a healthy singleton pregnancy
- Healthy pregnancies have been achieved after an embryo has been frozen for up to 10 years
By utilizing world class laboratory technology, New Hope Fertility Center’s pregnancy success rates through FET has increased substantially in recent years. That’s not all. Only high quality embryos are cryopreserve to be later transferred in future FET procedures. This success rate has made FETs an increasingly popular option to consider before considering a subsequent fresh IVF cycle. Bottom Line: With FET, couples can increase their chance of pregnancy per fresh egg retrieval and ultimately save money by avoiding the expense of another fresh IVF cycle.
Frozen Embryo Transfer Procedure
To begin the FET procedure, hormone medication is administered to suppress the woman’s pituitary gland and reduce the chances of unexpected ovulation. Estrogen acts to thicken and mature the uterine lining – like the natural estrogen produced by a developing egg follicle during a normal menstrual cycle.
During estrogen administration, monitoring of the uterine lining is required.
- Transvaginal ultrasound for the doctor to evaluate the thickness of the uterine lining
- Blood tests for the doctor to evaluate the level of estrogen in the blood
Double Benefit of FET: Monitoring for timing of transfer during a FET cycle is more flexible than in a fresh IVF cycle. The FET procedure is much less stressful on patients because the transfer date can be adjusted.
Progesterone is a medication administered in preparation for the FET to make the uterine lining receptive to the implantation of the embryo.
- Progesterone matures the uterine lining
- Progesterone creates a window of implantation in anticipation of a set FET date
- Lupron injections are ceased upon the beginning of progesterone administration
- Embryos are scheduled for thaw in the laboratory
- FET is scheduled on a set date
- Progesterone is continued daily to help prepare the patient’s uterine lining for implantation of the fertilized egg – the embryo
- After the embryo transfer, a pregnancy test is scheduled on a date prescribed by the doctor through a blood draw
Healthy pregnancies have been achieved after an embryo has been frozen for up to 10 years. Pregnancy success through FETs is determined by the quality of the frozen embryo.
Single Embryo Transfers
Dr. John Zhang – founder of New Hope Fertility Center – promotes the practice of Single Embryo Transfer (SET) to reduce health risks associated with multiple pregnancies and births. Cryopreservation of surplus embryos for future FET procedures is encouraged by the Doctor – in lieu of repeated, expensive fresh IVF cycles.
Pioneering Vitrification Method of Freezing Embryos
The flash-freezing technique of vitrification makes it possible to ready fresh embryos rapidly for cryopreservation. Using the vitrification method, embryos freeze quickly and damaging ice crystals do not form between cells. New Hope Fertility Center is a leader in embryo freezing. Dr. John Zhang was one of the first doctors in the United States to implement the vitrification method of embryo freezing.
It is important to work with a fertility doctor having the experience required to design a customized IVF and FET treatment plan meeting your personal and medical needs. To schedule your initial consultation with Dr. John Zhang at New Hope Fertility Center, call 917.525.5496.
The Key Role Fertility Medications Play in Your IVF Cycle

 Timing is of the essence when it comes to the administration of fertility medications during every infertility treatment cycle – especially IVF. Why does timing matter so much? Your fertility doctor must have the specialization to know when your fertility medication regimens must be adjusted: increased, decreased, or stopped altogether. Look: IVF pregnancy success rates are increased when your fertility team has the talent for managing medication therapies with unrivaled precision.
Timing is of the essence when it comes to the administration of fertility medications during every infertility treatment cycle – especially IVF. Why does timing matter so much? Your fertility doctor must have the specialization to know when your fertility medication regimens must be adjusted: increased, decreased, or stopped altogether. Look: IVF pregnancy success rates are increased when your fertility team has the talent for managing medication therapies with unrivaled precision.
Strategic Administration of Fertility Medications
Dr. John Zhang at New Hope Fertility Center has the education, training, and clinical experience to determine precisely how long his patients should remain on a certain medication therapy. As a patient who is committed to investing your time and resources into getting pregnant, you must become well-informed about fertility medications. It can’t be emphasized enough. Every fertility drug is specifically designed for strategic administration during a woman’s IVF cycle. These medications are a very important component of the IVF cycle process and are determinative of pregnancy success.
That’s not all. The Doctor’s standard of care encompasses the detailed explanation of the important role of fertility medications:
- Prepare the patient’s body for treatment
- Control the patient’s natural ovulation function
Personalized IVF Care
It is important to work with a fertility care team having the experience to accurately prescribe and regulate the fertility medications prescribed as part of your infertility treatment cycle.
- Timed Intercourse with medical assistance
- Intrauterine Insemination (IUI)
- Conventional IVF
- Mini-IVF™
- Natural IVF
Common IVF Fertility Medications
Fertility medications commonly used during IVF cycles:
- Lupron® is the trade name for an injectable leuprolide acetate used to prevent premature ovulation. Lupron® gives the patient’s body the opportunity to produce a higher number of quality eggs during the IVF cycle. Lupron® essentially switches off the pituitary gland in terms of its ability to produce follicle stimulating hormones and luteinizing hormones. Brand name Ganirelix may be used instead.
- Gonadotropins are follicle stimulating hormone (FSH) injections. Brand names including Bravelle®, Follistim®, Menopur®, and Gonal-F®, stimulate the follicles that contain the eggs during the stimulation phase of the IVF cycle.
- Human chorionic gonadotropin (hCG) are injections used during ovarian stimulation to trigger the maturation of the eggs and prepare them for retrieval. These hCG injections simulate the effects that an increase in luteinizing hormone would have in a woman going through natural ovulation. Lupron can also be used with certain stimulation protocols.
- Progesterone thickens a woman’s uterine lining to sustain a pregnancy when embryo implantation occurs. During IVF, a woman’s body generally does not produce enough progesterone to create a sufficiently thick uterine lining to support early embryo implantation. In this case, progesterone in various forms can be administered to augment the body’s natural supply until the placenta is able to produce adequate amounts.
Timed Intercourse and Intrauterine Insemination (IUI) Fertility Medications
When a couple is experiencing unexplained infertility despite normal reproductive health, medically supervised timed intercourse or IUI are usually recommended to increase the chances of pregnancy. IUI is the best and lowest cost approach to becoming pregnant when timed intercourse at home fails.
Clomid (Clomiphene Citrate) vs. Femara (Letrozole)
The fertility drug clomiphene citrate – brand named Clomid – is an oral medication used to stimulate a woman’s monthly egg production and increase her chances of pregnancy. Ovulation of multiple eggs is timed with the insemination of a concentrated amount of sperm into the uterus via a woman’s cervix – similar to a Pap smear.
A 2015 study published in the New England Journal of Medicine tested and compared two common fertility drugs stimulating multiple egg production – Clomid v. Femara. Clomid achieved a birth rate of 23 percent, while Femara (generic Letrozole – an aromatase inhibitor) only 18 percent. The study found that Letrozole offered no advantages over Clomid treatment and increased the chance of multiple pregnancy by up to four times. The researchers concluded that Clomid is the most effective medication for stimulating ovaries and increasing the chances of a healthy pregnancy for couples with unexplained infertility.
IVF Fertility Medication Administration Expertise
It is important to work with a fertility doctor having the experience required to design a customized IVF treatment plan meeting your personal and medical needs. To schedule your initial consultation with Dr. John Zhang at New Hope Fertility NYC – or – call 917.525.5496.
Unique Uterine Lining Thickening Treatment
 Patients who have been referred to gestational surrogacy can now renew their hope of becoming pregnant and carrying a baby to full term themselves. At New Hope Fertility Center, we have unique expertise in optimizing the thickness of a woman’s uterine lining for successful embryo implantation and fetal growth.
Patients who have been referred to gestational surrogacy can now renew their hope of becoming pregnant and carrying a baby to full term themselves. At New Hope Fertility Center, we have unique expertise in optimizing the thickness of a woman’s uterine lining for successful embryo implantation and fetal growth.
Uterine Lining Thickening
When a woman’s uterine lining is too thin for an embryo to attach and thrive into a fetus, she is diagnosed as having a thin endometrial lining.
Embryo Implantation Failure
Embryo implantation failure is the inability of an embryo to attach to the lining of the uterus. Most failed implantations are due to poor embryo quality. However, good quality embryo implantation failure can occur due to poor endometrial receptivity when a woman suffers from a constantly thin endometrium.
Constantly Thin Endometrium
Pregnancy and live birth success rates rise substantially with increased endometrial thickness – independent of patient age and embryo quality factors.
- Embryo implantation rates are highest when the endometrial lining has a thickness of 9 mm or greater
- An endometrial lining thickness of 8 mm is adequate for embryo implantation
- A constantly thin endometrial lining – 7 mm or less – is cause for concern of a potential failed cycle
- Less than 6 mm – there is almost no chance of a pregnancy
Treatment to Increase Thickness to the Endometrial Lining
An unexplained constantly thin endometrial lining can be corrected through estrogen treatments supplemented with Viagra.
- Estrogen Treatment. During a typical IVF cycle, additional estrogen treatment in the form of progesterone vaginal suppositories and/or injections can be prescribed to thicken the uterine lining in preparation for embryo implantation after transfer. Estrogen supplementation improves the overall endometrial lining thickness and increases the chances of a successful IVF pregnancy outcome.
- Viagra Treatment. Studies have shown that Viagra (Sildenafil) increases blood flow to the uterus – similar to how it increases penile blood flow in men suffering from erectile dysfunction. The increase in blood flow uterus is hoped to deliver more estrogen to the uterine lining. Viagra vaginal suppositories may be prescribed when the endometrial lining is constantly thin despite estrogen treatment.
PGS/NGS Increases Your IVF Pregnancy Success Rate By 30 Percent

 Genetic screening of embryos in vitro has increased yearly IVF pregnancy success rates at New Hope Fertility Center by 30 percent. By checking out this data, you can get an idea of your average chance of pregnancy success through IVF. Look: PGS/NGS is recommended because this technology is proven to increase a patient’s average chances of pregnancy success. Why does this matter? All IVF success rates vary per the context of patient and treatment protocol characteristics. Bonus: PGS/NGS identifies the gender of your embryos so that you can plan and balance the sexes of your children.
Genetic screening of embryos in vitro has increased yearly IVF pregnancy success rates at New Hope Fertility Center by 30 percent. By checking out this data, you can get an idea of your average chance of pregnancy success through IVF. Look: PGS/NGS is recommended because this technology is proven to increase a patient’s average chances of pregnancy success. Why does this matter? All IVF success rates vary per the context of patient and treatment protocol characteristics. Bonus: PGS/NGS identifies the gender of your embryos so that you can plan and balance the sexes of your children.
IVF Candidates for Genetic Screening
We typically recommend genetic screening in conjunction with IVF for patients meeting one or more of the following categories.
- Age 35 and older
- History of previous pregnancies
- History of miscarriages
- History of failed IVF cycles – fresh and frozen transfers
When a woman reaches an advanced maternal age – over 35 – her chances for conceiving a baby having chromosomal abnormalities increase.
Why is this important? Low quality embryos:
- Reduce pregnancy success rates
- Increase miscarriage rates
- Increase chances for birth defects
PGS/NGS Technology
There are a number of genetic conditions that can adversely alter the course of life – both for baby and parents. PGS and NGS can be performed on each embryo developing in vitro – in the lab.
PGS/NGS is used to identify the most suitable and healthiest embryo(s) to transfer. This genetic screening technology detects chromosomal deficiencies in embryos – aneuploidy – an extra or missing chromosome.Read more: PGS/NGS Increases Your IVF Pregnancy Success Rate By 30 Percent
Is it Time for You to See a Fertility Doctor?

 If you are under 35 and have not been able to get pregnant after having regular, unprotected sexual intercourse for at one year, you should see a fertility doctor. For women over 35, the time period for trying to get pregnant naturally is shortened to six months. Look: A woman’s fertility is dependent upon her overall health, wellness and lifestyle choices. Many women suffering from infertility use up too much valuable time trying to conceive naturally when there is a simple medical solution to their problem. Bottom Line: Don’t delay treatment.
If you are under 35 and have not been able to get pregnant after having regular, unprotected sexual intercourse for at one year, you should see a fertility doctor. For women over 35, the time period for trying to get pregnant naturally is shortened to six months. Look: A woman’s fertility is dependent upon her overall health, wellness and lifestyle choices. Many women suffering from infertility use up too much valuable time trying to conceive naturally when there is a simple medical solution to their problem. Bottom Line: Don’t delay treatment.
When to See a Fertility Doctor
Infertility can be difficult to diagnose. The sooner you seek help from a fertility doctor, the less time you will waste trying to get pregnant.
- A woman’s peak fertility years are in her 20s to mid-30s
- Women in their peak fertility years have a 20 percent chance of pregnancy every month
- A woman’s fertility level begins to decline after 30 and there is a precipitous drop after she turns 35
- Women over 40 only have about a 5 percent chance of getting pregnant during any given month
Symptoms of Infertility
Are you experiencing any of these symptoms?
- Inability to get pregnant
- Menstrual cycle lasting too long – over 35 days
- Too short of a menstrual cycle – under 21 days
- Irregular menstrual cycle
- Absent menstrual cycle
Common Causes of Female-Factor Infertility
You may be suffering from one of these medical conditions:
- Failure to ovulate
- Irregular ovulation
- Uterine fibroids
- Ovarian cysts
- Endometriosis
- Polycystic Ovarian Syndrome (PCOS)
- Blocked Fallopian tubes
- Abnormally shaped uterus or cervix
- Hormonal imbalance